What is Congestive Heart Failure?
The human heart performs the function of a centralized blood-pumping organ in the body. When this contractile function of the heart develops abnormalities such that it becomes incapable of meeting the oxygen requirements of the peripheral tissues, this disease phenomenon is termed as congestive cardiac failure. Heart failure has now become highlighted as a major non-communicable epidemic worldwide. In the U.S.A only, a total of 550,000 individuals develop this pathology each year.
Congestive heart failure constitutes a major burden of disease throughout the world as its morbidity and mortality rates continue to rise globally.
Pathophysiology
A failing heart can be the outcome of any structural and/or functional derangement of the cardiac musculature. Such disturbances mostly arise due to the following factors:
- Myocardial infarction (MI) or death of the cardiac muscles
- Hypertension
- Dysfunction (stenosis or regurgitation) of the heart valves
- Cardiac enlargement or cardiomyopathy
- Miscellaneous factors e.g., renal failure, anemia, etc.
An episode of heart attack or MI can lead to a permanent loss of considerable contractile myocardium following which there occurs a systolic heart failure (reduced stroke volume) where the heart muscles fail to generate the pressure essential for sustaining a normal cardiac output. In addition, a long-standing state of hypertension creates significantly increased blood pressure (increased afterload) within the major arteries arising from the heart. This puts a higher workload over the cardiac muscles which causes them to undergo hypertrophy and eventually leads to cardiac failure. Valvular heart disease and cardiomyopathy also constitute important mechanisms underlying cardiac failure (increased preload/afterload).
What is the end-result of heart failure?
Instead of pumping it out adequately, a poorly-functioning heart continues to fill up with blood. This leads to a substantial backflow of blood into the lungs and into the peripheral circulation where it causes edema.
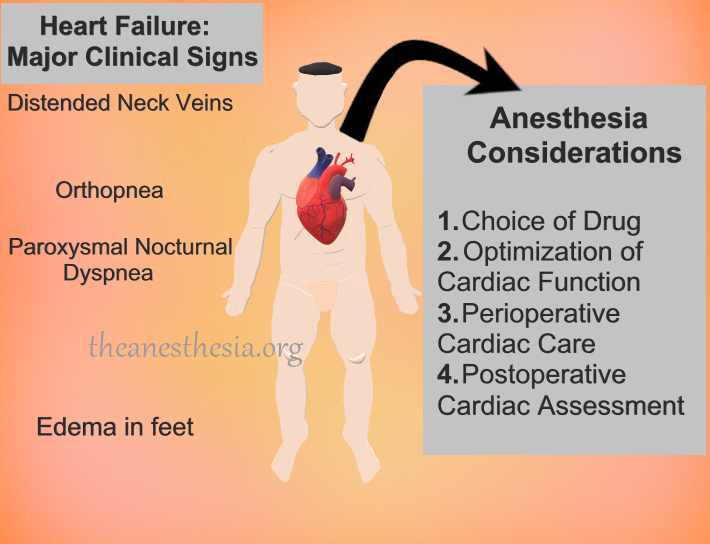
Clinical Manifestations
Following are some major clinical features of heart failure:
- Exercise-induced shortness of breath or dyspnea
- Dyspnea upon lying down flat for a few minutes (orthopnea)
- Waking up at night while gasping for breath (paroxysmal nocturnal dyspnea)
- Coughing and wheezing, especially at night
- Edema or swelling in the feet
- Distended neck veins
- Tiredness or generalized fatigue
- Palpitations
- Dizziness
Diagnosis
A meticulous physician would strongly speculate congestive heart failure, simply based on the patient’s clinical findings. However, a final diagnosis can be established with the aid of some notable diagnostic modalities. These include the following:
- On most occasions, suggesting a chest X-ray usually settles the diagnosis with the help of the following diagnostic findings: signs of pulmonary edema and increased cardiac size.
- Blood levels of brain natriuretic peptide (BNP) can become significantly elevated in chronic heart failure. This test is also being extensively used in securing a definite diagnosis of heart failure.
Treatment
Treatment of congestive heart failure requires a substantial modification of an individual’s dietary uptake as well as physical activity. In addition, a number of contributing risk factors have to be controlled optimally e.g., a good control over diabetes and hypertension. Pharmacological intervention consists of the following measures:
- Angiotensin-converting enzyme inhibitors (reduce afterload)
- Diuretic drugs (reduce preload)
- Beta-blockers (reduce cardiac contractility)
Anesthesia Considerations
In the event of elective surgery, patients diagnosed with congestive heart disease pose a major anesthesia risk. Therefore, it is customary to screen all the patients who are due for an elective surgical procedure for any clinical signs of heart failure. If any sign of heart disease is evident on chest X-ray, such a patient population should be cautiously assessed for any major cardiovascular complications in the perioperative period, or in worst cases, the surgery can be aborted.
The main goal of anesthesia team must be to avoid myocardial depression. The following are a few important measures to be adopted during anesthesia administration:
- Anesthesia drugs
The most ideal candidate must be selected for anesthesia induction and maintenance. As the inhalational agents are known to alter cardiac contractility, intravenous (IV) drugs may be preferred. These include IV propofol and etomidate. Opioid analgesics (e.g., remifentanil) can also be useful. Overdosing on any agent should be best avoided.
- Perioperative Monitoring of heart
Direct arterial catheterization may be carried out for monitoring blood pressure. In addition, transoesophageal echocardiography can also be a reliable tool for the evaluation of cardiac physiology in the perioperative period.
- Optimization of heart contractility
Heart rate should be continually monitored and if necessary, stimulating agents (e.g., dobutamine or dopamine) can be administered to boost the cardiac output.
- Postoperative evaluation
Finally, a meticulous postoperative cardiac care will help a patient undergo speedy recovery from the stress of surgery.
Key Points
- Congestive heart failure can lead to a significantly higher mortality rate during a surgical intervention.
- The cardiac performance of such patients must be optimized prior to operative intervention.
References
- Figueroa MS, Peters JI. Congestive heart failure: Diagnosis, pathophysiology, therapy, and implications for respiratory care. Respir Care. 2006;51(4):403-412.
- de Freitas EV, Batlouni M, Gamarsky R. Heart failure in the elderly. J Geriatr Cardiol. 2012;9(2):101-107.
- Roger VL. Epidemiology of heart failure. Circ Res. 2013;113(6):646-659.
- Magner JJ, Royston D. Heart failure. Br J Anaesth. 2004;93(1):74-85.
