What is meant by Cardiac Performance?
Cardiac performance refers to the cardiac output, which is defined as the total volume of blood pumped by the heart into circulation per minute. An efficient cardiac output is essential for adequately sustaining the peripheral organ perfusion. Moreover, the cardiac output needs to be adjusted whenever a person is subjected to physical stress, and this becomes possible only through its modulation by the neuroendocrine system.
The World Health Organization (WHO) has identified the cardiovascular disease as the most prevalent cause of mortality worldwide which necessitates understanding the concept of cardiac output so as to comprehend the pathophysiology of various cardiovascular disorders.
Normal Physiology of Cardiac Output
Cardiac output is a major determinant of the hemodynamic performance of the body. It is dependent upon two cardiovascular parameters, as shown below:
- Heart Rate
- Stroke Volume
Cardiac output (stroke volume ×heart rate)
Cardiac rhythm is generated from the sinoatrial (SA) node of the heart. The heart rate implies the exact number of heartbeats experienced per minute whereas the stroke volume refers to the total volume of blood ejected by the left ventricle during each beat. Normal heart rate stands between 60-100 beats per minute while normal stroke volume equals 70 milliliters. The product of these two factors gives us the cardiac output which on average, stands at 5 liters per minute. However, this may become 5-7 times higher during extreme physical exertion.
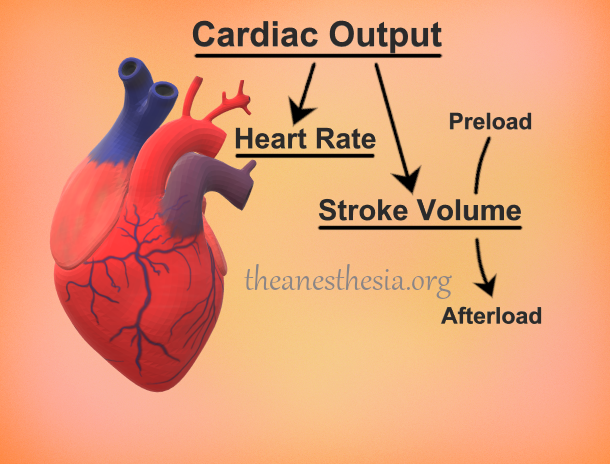
Preload and Afterload: Determinants of Cardiac Output
During each cardiac cycle, heart muscles undergo two different phases i.e., systole and diastole. Systole is when the heart muscles contract while diastole is when the myocardium undergoes relaxation.
Preload is determined by the volume of blood present within the left ventricle prior to the systolic contraction of the heart. The greater the ventricular volume, the higher the amount of stretch created in the ventricular musculature, and this results in an increased cardiac output. This mechanism has been termed as Frank-Starling law. Preload, also referred to as left ventricular end-diastolic pressure (LVEDP), is the volume at the end of the diastole ventricular stretch.
On the contrary, afterload is described as the peripheral arterial resistance which the left ventricle has to overcome during systole. Afterload is the amount of resistance that the heart must overcome in order to open the aortic valve and force the blood volume out into the systemic circulation, also known as systemic vascular resistance (SVR). The higher the resistance, the lesser the cardiac output. However, this can be overcome by potentiating cardiac contractility.
Neuroendocrine Modulation of Cardiac Output
Cardiac output can also be influenced as a result of a multitude of neurohormonal factors, some of which are stated below:
- Sympathetic and parasympathetic stimulation
- Direct actions of epinephrine
- Thyroid hormones
These factors can directly influence the contractility of the heart muscles. An increased contractility can help the heart get rid of an increased preload while it can also assist the left ventricle overcome a higher-than-normal afterload.
Pathophysiology
Cardiac output can become deranged through a variety of pathological factors. These mechanisms can negatively alter cardiac performance while their effects can become evident either instantaneously or may take months or even years. A few of these pathological conditions include:
- Essential hypertension
- Congestive heart failure
- Myocardial infarction due to coronary artery disease
- Valvular heart disease
- Cardiomyopathy
- Hypovolemic shock
- Cardiovascular thromboembolism
- Cardiac tamponade
- Drug-induced cardiotoxicity
Clinical Correlations
The Role of Ejection Fraction
As already illustrated, cardiac performance can be downgraded by a number of cardiovascular disorders. To correctly analyze the effect of these disease processes on cardiac function, ejection fraction can be measured by calculating the ratio of stroke volume to end-diastolic volume. This can be achieved by means of echocardiographic (ECHO) studies.
In case the ejection fraction is sustained around 0.6, this implies that the heart is contracting perfectly. However, this indicates the presence of a thick-walled left ventricle (e.g., cardiomyopathy) that fails to relax during cardiac cycle. This is known as diastolic failure of the heart. On the contrary, if the ejection fraction falls down to 0.4 or below, this signifies a systolic failure of the heart.
Clinical Management of Poor Cardiac Performance
Most of the conditions underlying a poor cardiac performance are directly correlated with some common risk factors. Alleviation of such risk factors is essential for achieving an optimal health. Following are some of these potential risk factors:
- Diabetes mellitus
- Hypertension
- Obesity
- Deranged lipid profile
- Smoking
All of the aforementioned risk factors can be modulated with the help of dietary changes and exercise intervention. A well-balanced and cautious lifestyle is at the “heart” of maintaining a healthy cardiac performance. In addition, other noninvasive interventions including a long-term pharmacotherapy may be advised for an efficacious management of chronic heart disease.
Conclusion
Cardiac performance is influenced by several factors all of which can be subjected to pathological mechanisms. However, with the help of careful intervention measures, cardiac machinery can be salvaged in the best possible manner.
References
- King J, Lowery DR. Physiology, Cardiac Output. [Updated 2020 Sep 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470455/
- Vincent JL. Understanding cardiac output. Crit Care. 2008;12(4):174.
- Gordan R, Gwathmey JK, Xie LH. Autonomic and endocrine control of cardiovascular function. World J Cardiol. 2015;7(4):204-214.
