Coronary Circulation: A Basic Introduction
The blood circulation of the heart has been a subject of immense interest, and various modern techniques have been devised to evaluate the condition of the coronary vasculature. The heart muscles are supplied blood by means of two major arteries that arise from the aorta. These include the right coronary artery (RCA) and the left coronary artery (LCA). The coronary circulation can be subjected to pathological insult through arteriosclerosis, which leads to narrowing or stenosis of these vessels. Hence, a timely diagnosis of any such life-threatening abnormality is of paramount importance for which a basic comprehension of their normal anatomy and physiology becomes essential.
Basic Anatomy
The coronary arteries can be broadly categorized as epicardial and intramuscular arteries. The epicardial vasculature is located superficially while the intramuscular vessels branch through the myocardium. The right and left coronary arteries originate from the proximal portion of the aortic trunk, commonly known as the sinus of Valsalva. The RCA gives rise to branches that supply the following major sites of the human heart:
- Right atrium
- The right ventricle and some part of the left ventricle
- Sinoatrial or SA node (the pacemaker of the heart)
- Atrioventricular (AV) node
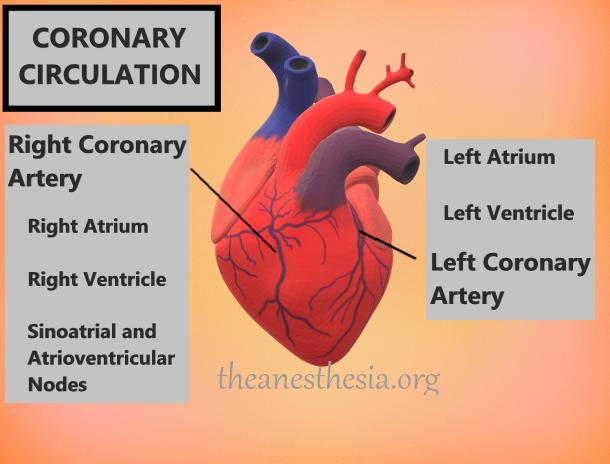
The LCA gives rise to two major branches: the left anterior descending artery (LADA) and left circumflex artery (LCXA). These provide oxygenation to the left side of the heart. The branches of the right and left coronary arteries possess a series of interconnecting vessels that serve as “collaterals”. These collateral vessels play a key role in reviving an area of the heart which has been subjected to ischemic insult.
Basic Physiology
The coronary circulation occurs in a biphasic manner with the blood flow increasing considerably during the diastolic phase as compared to systole. During the latter phase, the myocardium contracts vigorously following which the vascular channels inside the heart become compressed, thereby occluding any circulatory flow. In contrast, diastole allows relaxation of the myocardium, and hence, blood flow to the heart is restored. This nature of blood circulation is largely contradictory to the vessels found elsewhere as the systolic contraction of the heart increases peripheral blood flow.
At rest, diastole (~0.5 seconds) lasts longer than systole (~0.3 seconds). This allows an adequate flow of blood through the arterial circulation. However, an increased heart rate (tachycardia) results in an incomplete relaxation of the myocardium which reduces the total duration of diastole. This, in turn, diminishes the overall blood flow to the heart leading to a curtailed myocardial perfusion. This phenomenon depicts the vulnerability of patients with coronary artery disease (CAD) towards the development of myocardial infarction while experiencing exercise-induced tachycardia.
Autoregulation of Coronary Blood Flow
The cardiac workload is a major determinant of coronary circulation where the blood flow increases due to a steeply rising myocardial oxygen demand. During physical stress/exertion, ventricular muscles have to contract much more strenuously. This causes the muscle cells to derive a higher-than-normal blood flow from the coronary circulation. However, increasing the consumption of oxygen is not entirely sufficient for sustaining the myocardial contractility.
For this purpose, myocardial hypoxia induces the production of a number of chemicals that allow dilatation of the coronary arteries and hence, boost the overall supply of blood into the myocardium. Not only hypoxia but gradually accumulating concentration of carbon dioxide is also implicated in this process. Still, however, the exact mechanism underlying these changes in coronary blood flow is poorly understood.
Major contributors of Coronary Auto-regulation
1. Adenosine
Adenosine has long been considered as a possible mediator of coronary autoregulation. It has been proposed that a relative deficit of oxygen leads to the degradation of adenosine triphosphate (ATP) in the myocardial cells, and subsequently causes an accumulation of adenosine. The latter potentially acts as a vasodilator agent when released into the heart vessels. Adenosine has also been linked to restoring blood supply to the oxygen-deprived, ischemic myocardium.
2. Nitric Oxide
Nitric oxide is a key vasodilator molecule for the peripheral blood vessels. In a similar manner, its role has also been documented in the maintenance of coronary circulation at rest as well as during increased physical activity.
3. Prostaglandins
Prostaglandins are implicated in a multitude of important functions throughout the body. Prostacyclins, a subtype of these molecules, play an essential role in vasodilatation and thus, help maintain coronary blood flow.
4. Autonomic Nervous System
Finally, the autonomic nervous system provides sympathetic innervation to the cardiac musculature and vessels. Stimulation of the alpha-adrenergic receptors which are distributed along the coronary vessels mediates an efficient regulation of the coronary blood flow.
5. Myogenic Response of Vessels
Other factors which regulate coronary blood flow include the myogenic mechanism of blood vessels which allows dilatation of the coronary arteries in response to reduced vascular flow and vice versa.
References
- Rehman S, Khan A, Rehman A. Physiology, Coronary Circulation. [Updated 2020 May 30]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482413/
- Ali N, Patel PA, Malkin CJ. Assessment of coronary physiology – the evidence and implications. Clin Med (Lond). 2019;19(5):364-368.
- Patel S. Normal and anomalous anatomy of the coronary arteries. Semin Roentgenol. 2008;43(2):100-112.
