Anesthesia Provider must be ready to address airway related complication while doing Non-OR Anesthesia Procedures. Most complications are desaturation, airway obstruction, apnea, hypoxemia, and Laryngospasm.
The goal of the anesthesia provider is to maintain a patent airway, ventilatory drive, and reflexes are preserved with minimal to no airway support during the procedures.
To maintain deeper anesthesia level and gas exchange anesthetist may require to use different modalities for airway management devices. Commonly used airway management device listed below.
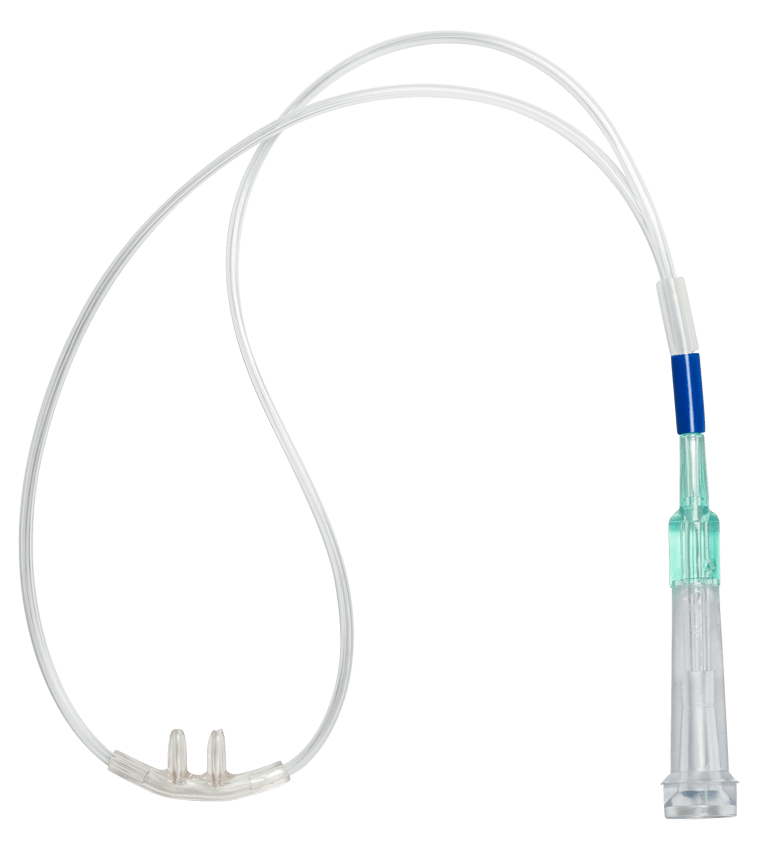
Nasal Cannula:
The traditional way of giving anesthesia with a nasal cannula and can provide a good amount of oxygen concentration to the patient if you have a patent airway. Generally, the nasal cannula can provide up to 44% of FI02. 1 Liter of oxygen provided 24% of FIO2 and each one-liter increase in flow increase 4% of FI02.

Higher the oxygen flow patient might go to have a dry nose, irritation, and nose bleed. If your patient required higher oxygen consider switching to a face mask.
Simple Face Masks: ( Venturi Mask )
A simple face mask can deliver higher oxygen concentration delivery of 40 to 60 percent. A minimum of 5 Liters of O2 flow is required in order to clear exhale gases from the mask also it can deliver up to 60% FIO2 at 10 Liters of flow.

Non Re-breather Masks: This mask can provide up to 100% FIO2 at 15 liters of the flow but commonly designed for oxygen support for various pulmonary disorders.
High Flow Nasal Oxygen (HFNO):
High flow nasal oxygen is used in spontaneous breathing patients and can deliver up to 100% FIO2, usually humidified and heated in -order to prevent mucosal dryness and to maintain the hydrated airway. High Flow nasal oxygen decreases the episode of desaturation but the biggest drawback is, it does not have the ability to monitor ETCO2, and a Transcutaneous C02 monitor can be used instead.
Two key companies are manufacturing these devices: Vapotherm which has a device capable of delivering flow rates of up to 50 liters/min, and Fisher Paykel which provides both the Optiflow and the AIRVO 2 devices capable of delivering flow rates of up to 60 liters/min.
Procedure Oxygen Mask:
According to POM Medical, this mask delivers approximately 80-90% Fio2, The POM claims the safest choice for endoscopy, bronchoscopy, conscious sedation, and is the #1 FDA approved mask for procedural sedation with proven sensitive respiratory rate tending via end-tidal Co2.

Nasal PAP Ventilation System:
Delivers positive airway pressure to stent open the upper airway, allowing for the preoperative delivery of positive pressure ventilation and oxygen for patients with a decreased level of consciousness. This nasal PAP ventilation device is available in medium and large sizes and is offered as a standalone mask with a head strap and as a system, kitted with a hyperinflation bag also compatible with anesthesia machine or Mapleson circuit.

Mask Adapter for Upper GI Endoscopy ( MAUGE Device):
This device is widely used in Europe, an adapter combined with regular anesthesia mask, proximal end connected either to Mapleson circuit or to an anesthesia machine and other port for endoscope entry. Common caveats for this method are mask must be held to prevent the air leak.

Endoscopy Masks/ Bronchoscopy Masks:
Endoscopy masks are designed to allow easy insertion of an endoscope probe into the nose or mouth whilst administering an analgesic gas at the same time. There are three one-way valves positioned on the mask which provide easy access from either side of the patient. The masks are principally used for bronchoscopy procedures, and the analgesic gas is administered via the central 22mm port. These masks could also be used with patients undergoing a Transesophageal echocardiogram (TEE) procedure. This device is also known as Bronchoscopy Masks.

Oropharyngeal Airway or Bite Blocks:
The oral airway is otherwise called Guedel pattern airway or simply Guedel airway widely used in daily anesthesia practice. An oropharyngeal airway is an adjunct to the airway used to retain or open the airway by preventing the epiglottis from being blocked by the tongue. ⠀

Ventilating Bite Block:
This bite block has a central aperture for the introduction of the endoscope through an air-tight, removable diaphragm. Two 15 French connectors provide an interchangeable connection to a breathing system or allow insertion of a suction catheter. A soft flexible airway is designed to be inserted after sedation prevents gaging. An inflatable cuff surrounding the device allows the creation of an air-tight seal. Widely used for endoscopic retrograde cholangiopancreatography (ERCP)

Nasal Airway ( Nasopharyngeal airway):
A flexible soft tube is inserted into the nasal passage to the base of the tongue to allow airflow. Also, you can connect an ETT tube adapter at the end of the nasal airway and attached it to the Mapleson circuit, and give positive airway pressure. Common contraindication for placing nasal airway is anticoagulated patients, a nasal fracture, and nasal deformity patients, and suspected cranial vault fracture patients. A common complication of placing nasal airway is epistaxis and aspiration of blood.

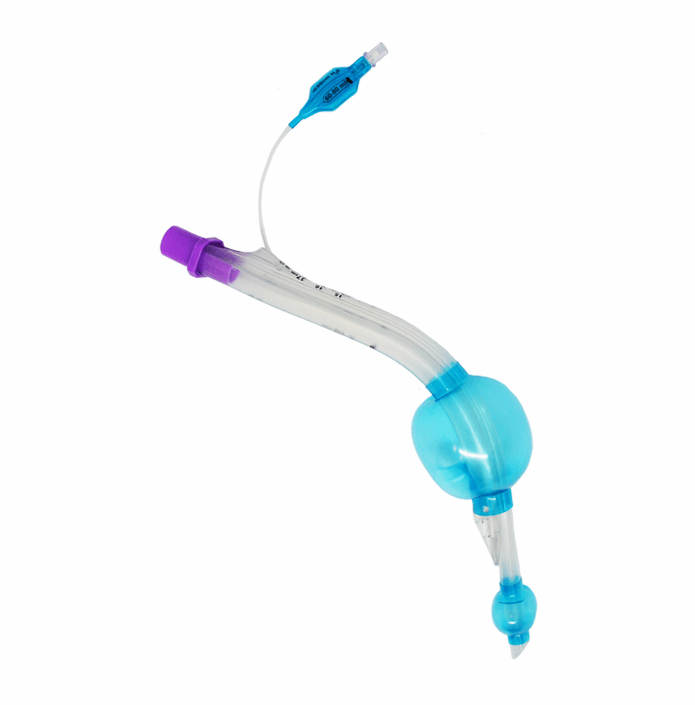
LMA Gastro:
The LMA Gastro Airway with Cuff From Teleflex is the first laryngeal mask specifically designed to enable clinicians to proactively manage their patients ‘airways while facilitating direct endoscopic access via the integrated endoscope channel. clinicians can monitor end-tidal CO2 for patient safety.

Gastro-Laryngeal tube:
Obtains and maintains control of airway patency during gastrointestinal endoscopic procedures. Use with adults under deep sedation or general anesthesia while maintaining spontaneous or assisted ventilation. Prevents and controls hypoventilation and desaturation. Eliminates the need for direct laryngoscopy or muscle relaxation. Enables capnometry and capnography. Protects airway from gastroesophageal reflux and inhalation of gastric content.
Summary:
Currently, minimally invasive diagnostics and therapeutic procedures are more performed outside the operating room due to the advancement of medical technology. The anesthetist is more dependent upon these devices to decrease incidents of complications and cut the cost of health care. No one device is superior to the other, choosing these devices is depended upon the patient’s condition and the anesthetist’s familiarity with the device.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4024697/